 |
George Kasali describes key factors that make Zambia’s health sector vulnerable to climate change, focusing on malaria and the impacts of floods and droughts. |
| He explores disease sensitivity to rainfall and temperature, focusing on malaria, and describes the health impacts of floods and droughts. He concludes that sustainable solutions to climate-related hazards, the mainstreaming of climate risk reduction and adaptation into national health plans, and research to fill the vast health and climate change knowledge gaps are essential. | |
| The author is a researcher with Energy and Environmental Concerns for Zambia. | |
Zambia is already saddled with a huge disease burden with over eight million clinical cases of malaria, diarrhoea, respiratory infections and other communicable but avoidable illnesses robbing the country of millions of productive hours each year. Zambia’s infant mortality rate is an enormous 112 per 1000 live births. In 2003, the average life expectancy was 39 years and Zambia ranked 163 out of 175 in the Human Development Index ( latest report). Climate change impacts are expected to be greater in developing countries like Zambia because of their geographical location, high dependence on natural resources and limited economic, financial, human and institutional capacity to effectively respond. Food shortages, drought and heavy rains are already commonplace in Zambia, and this situation has been worsened by the increased frequency and magnitude of climate variability in recent years.
Climate and climate change in Zambia
Zambia is a land-locked country in Southern Africa. In general, the year can be divided into two distinct halves, a dry half from May to October and a wet half from November to April. Average annual rainfall is 1001 millimetres, more than 90 per cent of which falls in the rainy season from November to March. July is the coldest month and October is the hottest.
Climate change is not expected to cause any new climatic events in Zambia, but rather to alter the long-term frequency, magnitude and intensity of current climate variability. Rainfall in the south and central parts of the country between 1970 and 2000 has tended to decrease, although floods have also been common. The first rain used to fall in October or the first week of November, but in recent years, the rainy season has tended to start a week or two later. Since the early 1980s, there has been a tendency towards the late onset and early withdrawal of the rainy season.
Since the early 1970s, there has been a modest warming in the cool season (June to August), with considerable warming (by about one degree Celsius) of the mean maximum temperature in the hot season (September to November), especially in northern areas. A tendency towards more extreme temperatures between 1970 and 2000 was observed throughout the country.
Future climate projections for Zambia up to the year 2070 predict more droughts and extreme temperatures in southern and central areas, and increasing rainfall in northern parts of the country. One climate model predicts a five to twenty per cent decrease in the length of the growing (rainy) season by the year 2050.
| Indicator | 1990/1992 | 2002/2003 | 2015 target |
|---|---|---|---|
| Proportion of people living in extreme poverty (%) | 58 | 46 | 29 |
| Proportion of people living with extreme hunger (%) | 25 | 28 | 12.5 |
| Under-five mortality rate per 1000 births | 191 (1992) | 168 | 63 |
| Infant mortality rate per 1000 births | 107 | 95 | 36 |
| Maternal mortality rate per 100,000 live births | 649 | 729 | 162 |
| Trends in HIV infection among antenatal clinic attendees (%) | 20 (1994) | 40 | 19 |
Zambia's disease burden
Existing disease burdens provide some measure of the adaptive capacity and vulnerability of the health sector in Zambia to the impacts of climate change. The top three reasons for visiting health facilities in Zambia in all age groups are malaria, respiratory infections (excluding pneumonia) and non-bloody diarrhoea.
Malaria is the largest cause of morbidity in Zambia and is a major public health problem accounting for nearly 40 per cent of all outpatient attendances at health facilities. The attendance figure rises to 50 per cent for children under five years. There are roughly four million clinical cases of malaria per year in Zambia and 50,000 deaths, including up to 20 per cent maternal mortality. The National Health Strategic Plan (2001 to 2005) aimed to reduce malaria incidence rates to 300 per 1000 people by the year 2005. This target has not yet been achieved, although levels are lower in urban areas with better access to treatment and control measures. Out of the rural areas, those in the north with higher altitudes and lower temperatures have the lowest morbidity rates.
Conversely, more people suffer and die from diarrhoea in urban than rural areas, with the highest incidence rates recorded for Lusaka Province, which houses Zambia’s capital city Lusaka. This may be attributed to overcrowding and poor sanitation.
Children under five years old carry much of the disease burden in Zambia. Incidence rates for malaria, respiratory infections, diarrhoea and pneumonia are 5.6, 5.1, 8.4 and 6.5 times higher, respectively, than rates for older people.
Zambia’s current disease burden is quite high, and achievement of the health-related Millennium Development Goal targets will require a drastic shift in health policy and investment. The table above shows the huge gap between the 2015 targets and existing human health indices. The National Health Strategic Plan (2006 to 2010) concludes that despite discrete and sustained improvements in some areas, Zambia is unlikely to meet most of the Millennium Development Goal targets by 2015.
Climate change impacts on health
Field surveys conducted under the National Adaptation Programme of Action on Climate Change ( 2.5Mb download)show that Zambia is vulnerable to droughts, floods, extreme heat and shifts in rainy season length. Almost all of these climate hazards will have a negative effect on health. Despite the increased frequency of these hazards in the past decade, Zambia has not yet developed any climate-informed policies for the health sector. This may in part be because of the limited available information on interactions between climate and disease in Zambia.
Disease sensitivity to rainfall
Some diseases are more sensitive to weather or climatic factors than others. Data on morbidity and mortality levels for various diseases in Chadiza and Mazabuka Districts in the Eastern and Southern Provinces, respectively, were collected from the Ministry of Health and the District Health Office in Mazabuka. These were then correlated with rainfall data for both districts collected from the Department of Meteorology in Lusaka. Daily or weekly health data were not accessible so monthly or three-monthly health data were used.
A simple linear relationship between rainfall and malaria is unlikely to occur due to confounding factors such as temperature, socio-economic conditions, population immunity levels, cultural habits and the impacts of existing interventions. A simple linear regression reveals, however, that between 1998 and 2005, malaria increased as rainfall increased in Chadiza and Mazabuka Districts. Rainfall distribution (which measures the total rainfall for a particular season adjusted for the number of rainy days) provided a better indicator of malaria prevalence than total rainfall. Studies from elsewhere in Zambia also found that malaria incidence in wet years was considerably higher than in dry years. Particularly notable are the reductions in malaria during the 2002 drought.
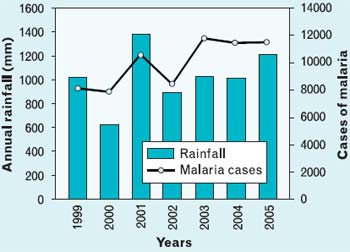 |
| Malaria prevalence and rainfall in Chadiza District |
The responses of diarrhoea and respiratory infections (that are not pneumonia) to rainfall are less clear. In the case of diarrhoea, this may be because in rural settings droughts reduce water supplies resulting in poor hygiene and less dilution of pathogens in water supplies resulting in more diarrhoea. In urban settings, however, more rainfall causes inadequate sanitation facilities to overflow or collapse thus carrying more pathogens to humans. Dysentery appears to increase with drought conditions, and pneumonia correlates with rainfall with similar trends to those of malaria.
Disease sensitivity to temperature
In order to explore the sensitivity of various diseases to temperature, monthly data on morbidity and mortality levels for Chikankata Hospital in Mazabuka District were collected from 1998 to 2002. Climate data were collected from Magoye meteorological station in the same district. Health data were analyzed with respect to the three distinctive seasons in Zambia.
Data confirm that there is increased morbidity (measured in terms of mean hospital admissions per month) from malaria and pneumonia during the hot rainy season. On the other hand, hot dry conditions favoured diarrhoea, non-pneumonia respiratory infections and dysentery. Morbidity due to HIV/AIDS is spread almost evenly over the three seasons (with slight increases seen during the cold dry season), perhaps because many infections can hospitalize a person with HIV/AIDS.
In the cases of malaria and diarrhoea, increased mortality accompanied increased morbidity according to season. In the cases of dysentery, pneumonia and respiratory infections that are not pneumonia, however, mortality peaked during the cool dry season, whilst morbidity peaked in other seasons. In short, cool dry conditions appear to stimulate death from these diseases.
The effect of temperature on malaria
Temperature, humidity and rainfall are the three main climatic factors that affect malaria transmission. The Malaria Risk in Africa (MARA) project has demonstrated that malaria is sensitive to temperature. Malaria parasites cease to develop in the mosquito vector when the temperature is below 16°C and the best conditions are when the mean temperature is between 20°C and 30°C, with a relative humidity of at least 60 per cent.
Areas such as Nyimba and Luangwa have a suitable climate for malaria and are classified as endemic by the MARA project. Here, malaria incidence rates are high and peak in the first quarter of the year. In MARA areas designated as marginal and epidemic, malaria incidences are relatively low. In marginal areas, incidences are perennially low with morbidity remaining fairly stable because contact between humans and the mosquito vector is minimal throughout the year. In epidemic-prone areas, such as Mpika in the Northern Province, malaria incidence is low for most of the year when climatic conditions do not favour mosquitoes. This lowers population immunity, which means epidemics can occur. In the first quarter of the year, malaria outbreaks begin to occur and incidence rates practically double. Climatic conditions and population immunity are both crucial factors in the genesis of epidemics.
It is evident that in Zambia the distribution and transmission of malaria are functions of both temperature and altitude. High-altitude areas above 1200 metres with mild temperatures constitute the marginal and epidemic malaria areas, while the hot low-lying areas provide suitable climatic conditions for malaria to be endemic. Generally, malaria is stable in the valleys and unstable on the plateaus and higher grounds, which are mostly in central and northern parts of the country.
Health impacts of droughts
Climate disasters are now an annual occurrence in Zambia, ravaging livelihoods and disrupting the economy. Zambia and the entire southern African region experienced drought during the 2004/2005 agricultural season. Two thirds of Zambia, mainly the Southern, Eastern and Western provinces, experienced prolonged dry spells resulting in irreversible damage to most crops, including drought-tolerant crops such as cotton and tobacco. In areas affected by drought, cereal (staple food) production losses ranged from 30 to 80 per cent with an average of 56 per cent. Some 1,232,661 people needed food assistance in affected districts. Some of the affected districts continued receiving food aid until June 2006.
The prevalence of child malnutrition, as measured by a child’s mid/upper arm circumference, was an average of 15.5 per cent. Between 3.2 and 6.9 per cent of children were at a high risk of mortality, and 51 per cent of children had an inappropriate diet diversity score. These areas historically suffer from chronic food shortages and poor dietary intake, with stunting (an indicator of chronic malnutrition) levels of between 40 and 59 per cent. More climatic extremes will worsen people’s existing poor nutritional status.
In one survey in a drought-affected area, 43 per cent, 62.6 per cent and 48.8 per cent of children had suffered from diarrhoea, a fever or a cough, respectively, in the week prior to the survey. About 20.7 per cent of adults in the survey area had been chronically ill for more than three months during the 12 months prior to the survey. Amongst these, 6.4 per cent were household heads. Some 51 per cent of those surveyed had experienced the drying up of water sources. Water supplies for livestock was also a key concern. Additional hazards to which the people in drought-affected areas were subjected included increases in conflict between humans and wild animals and increases in crop and livestock diseases. More climatic extremes will act as an additional burden on the health and livelihoods of those affected.
Health impacts of floods
Zambia experienced excessive rainfall during the 2005/2006 and 2006/2007 rainy seasons that caused widespread flooding in most parts of the country. These floods had many health-related impacts. A total of 1,443,583 people in 41 districts were affected by floods and required assistance in the form of rehabilitation of their houses, latrines, water wells, schools, clinics, roads and other infrastructure over the following year. The lives and livelihoods of 295,148 people were directly threatened, all of whom required urgent help, especially with emergency food relief.
The floods destroyed 10,954 houses leaving 17,172 people needing emergency shelter. There was a high risk of water contamination, especially from faecal matter, in 78 per cent of affected areas because the floods led to the collapse of toilets and flooding of unprotected shallow wells. This affected 1,012,540 people. Some 14 districts (or 288,532 people) were at high risk of malaria outbreaks. Over 5000 cases of and 137 deaths due to cholera were recorded in Lusaka, and outbreaks of rabies, the plague and trypanosomiasis occurred in some areas.
The floods negatively affected the education sector, with damage to classroom blocks, staff houses and toilets of up to 160 schools disrupting the education of about 150,000 children. On the other hand, receding water left enough moisture and nutrients to allow dry season crop cultivation in some areas.
 |
|
Lisutu, Zambia
© Richard Lord/UMCOR |
Zambia’s key vulnerabilities
Zambia’s health sector is very vulnerable to climate change. Several factors influence the extent to which vulnerable populations are exposed to climate change-related health risks. These factors include the state of health-care delivery systems, provision of water supplies and sanitation, and chronic poverty, food insecurity and nutrition.
The healthcare system in Zambia comprises of government, mission (churches), industrial and private sector health facilities. In 2002, the availability of these facilities was an average of one hospital per 100,000 people, one health centre per 8000 people and one health post per 500,000 people. This shortage of health facilities poses a serious constraint to accessing health services in Zambia.
In urban areas, 99 per cent of households are within five kilometres of a health facility while this figure is only 50 per cent for rural areas. Flood damage to roads and bridges and illness itself can seriously limit people’s ability to reach distant health facilities.
Health institutions are grossly understaffed. With a projected population of 11,297,304 (for 2006), the average doctor to person ratio is about 1:16,000 while the average nurse to person ratio is about 1:1900. The World Health Organization recommends ratios of 1:5000 and 1:700 for doctors and nurses, respectively.
Supplies of essential drugs and medical equipment pose another challenge to Zambia’s health system. Over the past four years, supplies have been erratic with as much as 50 per cent of essential drugs being out of stock.
Access to safe water supplies in Zambia in 2000 was estimated at 86 and 37 per cent for urban and rural populations, respectively. For sanitation, these estimates were 33 and four per cent for urban and rural areas, respectively. In shanty compounds, which house 50 to 70 per cent of urban inhabitants, however, at least 56 per cent of the population do not have access to safe water supplies and as much as 90 per cent of people have no access to satisfactory sanitation facilities. Water shortages during droughts dramatically reduce personal hygiene while floods overwhelm pit-latrines and contaminate water sources. Under such conditions, the proliferation of disease is unavoidable.
Poverty levels also serve to increase risk. In 2004, 68 per cent of Zambia’s 10.9 million people (as recorded by the 2000 census) lived on less than US$1 per day. Amongst these, 53 per cent were extremely poor. In rural areas, the overall poverty rate was 78 per cent with 52 per cent living in extreme poverty. In 2001, about 72 per cent of women in rural areas reported a lack of money for treatment or transport to a health facility. Total government expenditure on healthcare as percentage of Gross Domestic Product also fell from six per cent in 1997 to 1.5 per cent in 2005.
Some 70 per cent of Zambia’s population is food insecure. Their poor nutritional status has been attributed to unaffordable food prices, unsteady availability, livelihoods instability and inadequate diet diversity amongst other causes. Floods and droughts exacerbate food insecurity and malnutrition.
Vulnerability to extreme climatic events is a function of geographical and socio-economic factors. For example, malaria affects people in valley areas, the eastern provinces and wetland areas most. Vulnerable groups include children, pregnant women, those living with HIV/AIDS, riverine communities and fisherfolk. In riverine areas, for example, government programmes provide subsidized insecticide-treated nets to prevent malaria, but many fisherfolk use the nets for catching fish.
Conclusions
Zambia is currently saddled with a heavy burden of communicable climate-sensitive diseases. It is also very vulnerable to the impacts of climate variability and extreme weather events like droughts and floods. Climate models have projected that these extreme conditions will persist in the future. This study has shown that floods and droughts can increase disease levels in some affected areas by as much as 400 per cent. Zambia clearly needs to find sustainable solutions to hazards associated with extreme climatic events and must start now to mainstream climate risk reduction and adaptation into national health strategic plans and programmes. Vulnerable populations and localities must be targeted. If this does not occur immediately, the health targets of the Millennium Development Goals will not be met.
Research is also needed to fill the vast knowledge gaps relating to health issues associated with climate variability and change in Zambia. It is only through a better understanding of the interactions between climate and health that effective strategies, policies and measures for coping with climate variability and change can develop.
Acknowledgement
This research was conducted under the Capacity Strengthening of Least Developed Countries for Adaptation to Climate Change Programme.
Further information
George Kasali, Energy and Environmental Concerns for Zambia, PO Box 51288, Lusaka, Zambia. Fax: +260-1-252339. Email: kasali_george@yahoo.com.
On the Web
A number of World Health Organization publications on climate change are available.