Tiempo Climate Cyberlibrary
Health Impacts in Poor Nations
- Tiempo archive
- Complete issues
- Selected articles
- Cartoons
- Climate treaty
- Latest news
- Secretariat
- National reports
- IPCC
About the Cyberlibrary
The Tiempo Climate Cyberlibrary was developed by Mick Kelly and Sarah Granich on behalf of the Stockholm Environment Institute and the International Institute for Environment and Development, with sponsorship from the Swedish International Development Cooperation Agency.
While every effort is made to ensure that information on this site, and on other sites that are referenced here, is accurate, no liability for loss or damage resulting from use of this information can be accepted.
 |
Hannah Reid describes the range of direct and indirect impacts that climate change could have on health in poorer countries. |
| Direct impacts include heat stress and the effects of disasters, whereas indirect impacts include effects on the incidence of vector-borne diseases, like malaria, and food- and water-borne diseases. Impacts will be especially strong in poor nations where limited healthcare infrastructure, high disease burdens, regular droughts and floods, widespread poverty and a high dependence on natural resources compound vulnerability. | |
| The author is a senior researcher in the Climate Change Group at the International Institute for Environment and Development in the United Kingdom. She is also a Tiempo editor. | |
It is becoming increasingly clear that climate change and global warming will seriously affect human health around the world. From heat stress to food insecurity resulting from droughts and from malaria to the education of schoolchildren, the range of potential health problems sensitive to climate change is enormous.
Direct health impacts
The effects of climate change on health will be both direct and indirect. Direct effects include heat stress and the impact of extreme weather events, including those that fall beneath the threshold for what is defined as a "disaster". Such events will result in more frequent humanitarian emergencies, which will particularly affect people in high-risk areas such as coastal zones, river valleys and cities. Even in wealthy France, an estimated 11,435 people above the seasonal average died when a record-breaking heatwave struck in the first two weeks of August 2003. Responding, Health Minister Jean-François Mattei announced US$748 million in extra funding for hospital emergency services, a measure that would either be impossible or stretch government budgets to breaking point in much of Africa.
These direct effects will be especially powerful in the developing world, with its less-developed and poorly funded healthcare infrastructure. For example, floods in Bangladesh in 2004 caused about 800 deaths, while the cyclone of 1991 killed 138,000 people. Deaths caused by heat and cold extremes will rise in vulnerable groups, particularly those already suffering from heart and breathing problems, the very young, the elderly and the frail. According to the World Health Organization (WHO), the United Nations Environment Programme (UNEP) and the World Meteorological Organization, at least 150,000 people die unnecessarily each year and there are 5.5 million disability-adjusted life years, (a standard WHO measure to compare disease burdens) as a direct result of global warming.
Indirect health impacts
Many indirect effects occur because of the close relationship between climatic conditions and insect and rodent populations. For example, climatic conditions strongly influence the range of vector-borne parasitic diseases like malaria and leishmaniasis.
| Vector | Disease |
|---|---|
| Mosquitoes | Malaria, filariasis, dengue fever, yellow fever, West Nile fever |
| Sandflies | Leishmaniasis |
| Triatomines | Chagas’ disease |
| Ixodes ticks | Lyme disease, tick-borne encephalitis |
| Tsetse flies | African trypanosomiasis |
| Blackflies | Onchocerciasis |
Malaria, which is already the second leading cause of death in the world for five- to 14-year-olds, is expected to reach unprecedented levels because of climate change. There are already between 300 and 500 million cases of malaria in the world each year, and it has been estimated that between 260 and 320 million more people are likely to find themselves living in areas with malaria potential by the year 2080.
Malaria is of particular concern in Africa where UNEP estimates that it already slows economic growth by up to 1.3 per cent each year. In one highland area of Rwanda, malaria incidence increased by 337 per cent in 1987. Some 80 per cent of this increase could be explained by changes in rainfall and temperature. Further changes in temperature and precipitation could trigger malaria epidemics at the current limits of the disease, both in altitude and latitude, where people lack immunity and the impact of the disease is, therefore, greater.
In South Africa, it is estimated that the area suitable for malaria will double and that 7.2 million people will be at risk from the disease - an increase of 5.2 million. In addition, flooding, which is likely to increase as the climate changes, could help mosquitoes breed, thus spreading malaria to otherwise dry areas. The Sahel region, which has suffered from drought in the past 30 years and has experienced a reduction in malaria transmission as a result, could be at renewed risk from a malaria epidemic.
 |
|
Finnish Red Cross emergency hospital, Pakistan
© Yassine Gaba/EC/ECHO |
Food-borne diseases are likely to increase as a result of warmer temperatures. Water-borne diseases may also increase because of extra demands on diminished water supplies, which will in turn increase the risk of contaminated supplies reaching the public. This is particularly worrying for countries such as Bangladesh where water-borne diseases are already responsible for 24 per cent of all deaths. Diarrhoeal diseases, including cholera and typhoid, may increase as a result of more frequent and severe floods and drought. For example, flooding caused by Hurricane Mitch in 1998 brought about a six-fold increase in cholera in Nicaragua.
Variations in extreme weather typically associated with the El Niño cycle are likely to become more common and more intense, and these will have a variety of knock-on health impacts. Spending on healthcare in Bolivia, Chile, Ecuador and Peru fell by ten per cent due to the fall in Gross National Product after the El Niño cycle in 1982/83, for example, and Ecuador, Peru and Bolivia suffered serious malaria epidemics. Following excessive rainfall related to El Niño in 1997, some ten per cent of all Peruvian healthcare facilities were damaged and droughts in Brazil sparked forest fires, the smoke from which was a major public health problem leading to large numbers of patients with respiratory problems visiting already overstretched health facilities. Cholera had been absent from Latin America for nearly a century when the first cases appeared in Peru following the 1991 El Niño. These cases were spread out over a 1000 kilometre long stretch of coastline as a result of an El Niño-related bloom of algae in the rivers, estuaries and on the ocean coastline, combined with poor hygiene and contaminated foods.
The association between climate change and HIV/AIDS is by no means direct, but it is insidiously real. In Africa, for example, AIDS lowers productivity as more and more farmers are infected and affected. Survivors have to spend time attending funerals, looking after orphans, or managing the estates of the deceased. Absenteeism from school and work is common. At the same time, unreliable rain patterns, which are becoming a permanent feature in some areas of Africa, have led to crop failures of such magnitude as to lead to severe malnutrition, which accelerates the negative effects of the disease and poverty. Girls suffer disproportionately as many are forced into early marriage or prostitution to help their families survive. Many rural folk migrate to towns where they are more likely to get infected.
Population movements resulting from drought and environmental degradation can also provoke migration. People forced to leave their home and land may be faced with unsanitary refugee camps with a multitude of associated health problems.
 |
|
Medical assistance project, central Africa
© François Goemans/EC/ECHO |
Who is most vulnerable?
The Intergovernmental Panel on Climate Change is unequivocal: "The impacts of climate change will fall disproportionately upon developing countries and the poor persons within all countries, thereby exacerbating inequities in health status and access to adequate food, clean water and other resources." Climate change could also seriously undermine the health-related Millennium Development Goals to reduce child mortality, improve maternal health and combat HIV/AIDS, malaria and other diseases.
Poor communities in Africa are likely to be particularly vulnerable. Estimates by Christian Aid suggest that 182 million people in sub-Saharan Africa might die from diseases associated with climate change by the end of the century. Africa’s high vulnerability to the impacts of climate change is compounded by widespread poverty. Ongoing drought and floods, and a dependence on natural resources for rural livelihoods, in turn, increase vulnerability. Sub-Saharan Africa already supports a heavy disease burden including HIV/AIDS and malaria, cholera, dengue fever, yellow fever, encephalitis and haemorrhagic fever.
Knowledge gaps
Health is often neglected in the assessment of vulnerability and adaptation to climate change, but understanding of the impacts of climate change on health in developing nations is steadily improving. Several countries have conducted national assessments to determine their vulnerability to the impacts of climate change and evaluate the capacity of their health infrastructure to adapt. Despite this, much more concrete information is required for informed health and climate change-related decision making in poorer nations.
Much of the evidence gathered to date is anecdotal and, although clear trends are becoming increasingly apparent, it is difficult to isolate the influence that climate change might have on the spread of any one disease out of the multitude of other factors that will influence observed changes. Whilst counting the dead from a cyclone or heatwave can help give an indication of the scale of the direct impacts of climate change on health, assessing this is much more difficult for the indirect impacts where many more factors that could influence disease transmission need to be considered. Predicting what will happen in the future is even harder, especially in regions where it remains unclear what climate change impacts are likely to occur.
Even harder to estimate, but perhaps no less important, are the knock-on health impacts that climate change will have on poor and vulnerable communities. Malnutrition could increase as a result of declining food yields as the health of those who need to work the land to provide food and income for their families is compromised and some areas of land become unsuitable for crop production. Will people be able to rebuild communities damaged by climate-driven disasters if their health is poor? What will be the impact on the provision of education when the pool of healthy prospective teachers and students is diminished? Healthcare infrastructure in poor countries is already over-stretched, but to what extent could climate change-related disasters further drain public resources for healthcare? Climate change will not only affect people’s health in all the direct and indirect ways described earlier, but in doing so it will also hamper people’s ability to adapt to a changing, uncertain climate.
Acknowledgements
This article is based on material from the five Up in Smoke reports drawn up for different regions by Hannah Reid, Andrew Simms and other authors. The Up in Smoke reports (one global, two for Africa, one for Latin America and the Caribbean and one for Asia and the Pacific) are based on contributions from the Working Group on Climate Change and Development, otherwise known as the Up in Smoke coalition, and can be downloaded from the Up in Smoke website.
Further information
Hannah Reid, International Institute for Environment and Development, 3 Endsleigh Street, London WC1H 0DD, United Kingdom. Fax: +44-20-73882826. Email: hannah.reid@iied.org. Web: www.iied.org.
Bright Ideas

General Electric plans to cut solar installation costs by half

Project 90 by 2030 supports South African school children and managers reduce their carbon footprint through its Club programme

Bath & North East Somerset Council in the United Kingdom has installed smart LED carriageway lighting that automatically adjusts to light and traffic levels
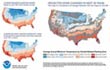
The United States National Oceanic and Atmospheric Administration and the American Public Gardens Association are mounting an educational exhibit at Longwood Gardens showing the link between temperature and planting zones

The energy-efficient Crowne Plaza Copenhagen Towers hotel is powered by renewable and sustainable sources, including integrated solar photovoltaics and guest-powered bicycles
El Hierro, one of the Canary Islands, plans to generate 80 per cent of its energy from renewable sources

The green roof on the Remarkables Primary School in New Zealand reduces stormwater runoff, provides insulation and doubles as an outdoor classroom

The Weather Info for All project aims to roll out up to five thousand automatic weather observation stations throughout Africa

SolSource turns its own waste heat into electricity or stores it in thermal fabrics, harnessing the sun's energy for cooking and electricity for low-income families

The Wave House uses vegetation for its architectural and environmental qualities, and especially in terms of thermal insulation

The Mbale compost-processing plant in Uganda produces cheaper fertilizer and reduces greenhouse gas emissions

At Casa Grande, Frito-Lay has reduced energy consumption by nearly a fifth since 2006 by, amongst other things, installing a heat recovery system to preheat cooking oil
Updated: May 15th 2015